Unlocking the Mystery of Sjögren's Syndrome
By: Heather Bancroft
Sjögren's Syndrome Foundation
Sjögren's (SHOW-grins) syndrome, an autoimmune disease in which the body’s immune system mistakenly attacks its own moisture-producing glands, often starts out as mystery. In fact, because of the variety of symptoms, it takes slightly more than six years, on average, to diagnose a Sjögren's syndrome patient.
Andrea Shafer was in her late 20s when she started having symptoms of Sjögren's. She noticed occasional pain in her legs and petechiae, a rash of red dots under the skin, on her legs. After a couple years of intermittent symptoms, she visited her family physician and was referred to a rheumatologist when her blood work suggested an autoimmune disorder. Eventually Andrea presented one of the more tell-tale signs of Sjögren's—dry eyes. In the end, it took Andrea about ten years to get a diagnosis of Sjögren's syndrome.
Because diagnosis can be such a challenge, Andrea says that she "would tell people to pursue that journey of connecting with the right provider, no matter how long it takes, no matter how many doctors you have to go to, even if you have to spend some of your own money to do it.
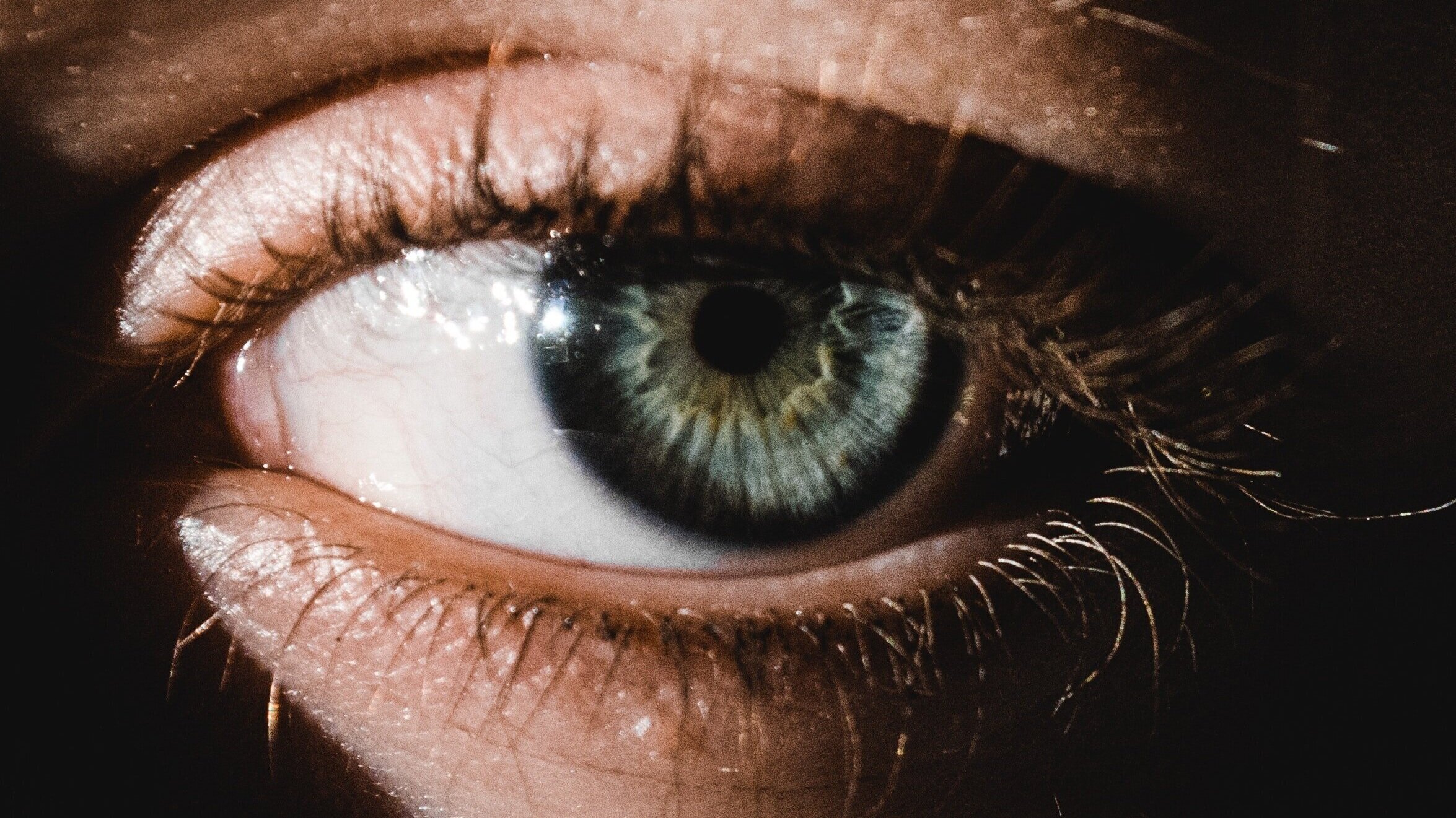
Symptoms of Sjögren's syndrome vary, but the hallmark symptoms are dry mouth and dry eyes. "People think of saliva as a trivial substance and tend to take it for granted, but when it is absent, it can have some life-altering consequences," says Frederick Vivino, M.D., a rheumatologist and director of the University of Pennsylvania Sjögren's Syndrome Clinic in Philadelphia. Patients may have trouble talking or may have to alter their diets to avoid spicy foods and use gravies to moisten drier foods. Severe dental decay can also occur. "With dry eyes, people often complain of a sandy or gritty feeling. Imagine what you feel like when you’re walking on the beach on a windy day and can’t quite get the sand out of your eyes," suggests Vivino. Other common symptoms include dryness of the skin, lungs, vaginal tissues, sinuses and gastrointestinal tract; joint and muscle pain; swollen glands; chronic fatigue and numbness.
Often times Sjögren's symptoms may come and go or don’t seem severe enough to warrant a visit to the doctor. Patients may talk to their dermatologist about a rash or their ophthalmologist about their dry eyes, but because the physicians are not interfacing or may be unfamiliar with Sjögren's, it may take a while for the pieces of the puzzle to come together.
The Sjögren's Syndrome Foundation (SSF) estimates that as many as four million Americans have Sjögren's syndrome, which affects women nine times more frequently than men. "It’s really a major women’s health problem that is largely being ignored by the medical community," acknowledges Vivino. "In the future, I’d certainly like to see a greater emphasis in the medical and dental school curriculums on the disease and its manifestations."
One of the obstacles to diagnosing Sjögren's is that there is not one simple test to identify it. Fortunately, within the past two years there has been a set of objective criteria developed to identify Sjögren's. Through subjective and objective measures which include patient interviews, blood work, a lip biopsy and tests that determine salivary and lacrimal (tear) function, doctors are able to determine if patients meet four of six criteria to make a diagnosis of Sjögren's.
The severity of symptoms among Sjögren's patients varies almost as much as the symptoms themselves. For some, their symptoms are so severe that chronic fatigue or the inability for those with dry eyes to work in front of a computer forces them to leave their careers and go on long-term disability. Shafer, 43, describes her condition as more of a nuisance. "It hasn’t stopped me from doing what I normally do, but, for instance, when I go to bed at night, I feel like I have a million things to do." This routine includes the application of eye ointments, taking vitamins for her eyes and an inhaled steroid, as well as Plaquenil, an anti-malarial medication which relieves fatigue and joint and muscle pain in many Sjögren's patients. Meticulous tooth brushing, flossing and fluoride applications also are important parts of the bedtime routine.
Kim Vaughn, a 45-year-old mother of two, has had numerous health problems since being diagnosed with Sjögren's syndrome fifteen years ago. In addition to suffering from mini strokes, arthritis and depression, she has had to have surgery on her sinuses as a result of fungal infection caused by dryness, and has to have her teeth cleaned every two to three months because of the decay caused by her dry mouth. "It’s more than dry eyes and dry mouth. It’s systemic—it affects your whole body," she says.
Vaughn has not slept a full night since learning she had Sjögren's, and finding the energy to meet the needs of her 10- and 15-year-old sons has been one of the hardest things for her. "Every day brings its own set of challenges, because I don’t know how I am going to feel. It‘s frustrating to have to take a nap in the middle of the day when there are so many other things you could be doing."
Vaughn, who is managing her symptoms through exercise and medication, acknowledges that there are many promising advancements on the horizon for patients, but admits that knowing that she is at increased risk of non-Hodgkin’s lymphoma scares her. Approximately one in 20 of those with Sjögren's syndrome will develop lymphoma, the majority non-Hodgkin’s lymphomas. Additionally, about 50 percent of Sjögren's patients have another autoimmune disorder like lupus or rheumatoid arthritis.
The exact cause of Sjögren's is unknown but it’s believed that people inherit genetic tendencies to develop an autoimmune disease and that environmental triggers, such as a virus, bacteria, or even chemical exposure could start the disease process. Sjögren's is a chronic disease, meaning that it lasts a lifetime—so treatments are designed to manage the symptoms, not address the underlying cause.
According to dentist Dr. Philip Fox, president of the SSF, there are now three prescription medications approved for use with Sjögren's, which include two drugs that stimulate salivary production and one to improve tear function. Other treatments include an exercise regimen, procedures to close ducts through which tears escape to retain moisture, over-the-counter moisture replacement products, aspirin and other non-steroidal anti-inflammatory drugs, steroids, and immunosuppressant drugs. Fox anticipates that the next five years in Sjögren’s research will be very exciting, "In the meantime, there are a lot of simple things one can do to minimize symptoms.," he says. "These are detailed in The Sjögren’s Syndrome Handbook, a publication of the Foundation."
For more information on Sjögren's syndrome, call the Sjögren's Syndrome Foundation at (800) 475-6473 or visit www.sjogrens.org.